February 11, 2026
Jim G. Whitcomb
Biological Indicators, Sterilization Modalities, Validation Requirements, Sterility Assurance Level (SAL), D-values, z-values, BIER Unit
Sterilization Validation Consulting, Biological Indicator Development, Fractional and Sublethal Studies, Bioburden Testing, Routine Sterility Testing
Several different modalities are available for the sterilization of medical devices. The chosen method requires validation to comply with current Good Manufacturing Practices (GMP) and to demonstrate the process renders the product free of viable microorganisms ensuring it produces product that meets requirements for a sterility claim. Since microorganisms are invisible to the naked eye, different techniques have been developed to monitor the survivability of microorganisms when exposed to a sterilization process.
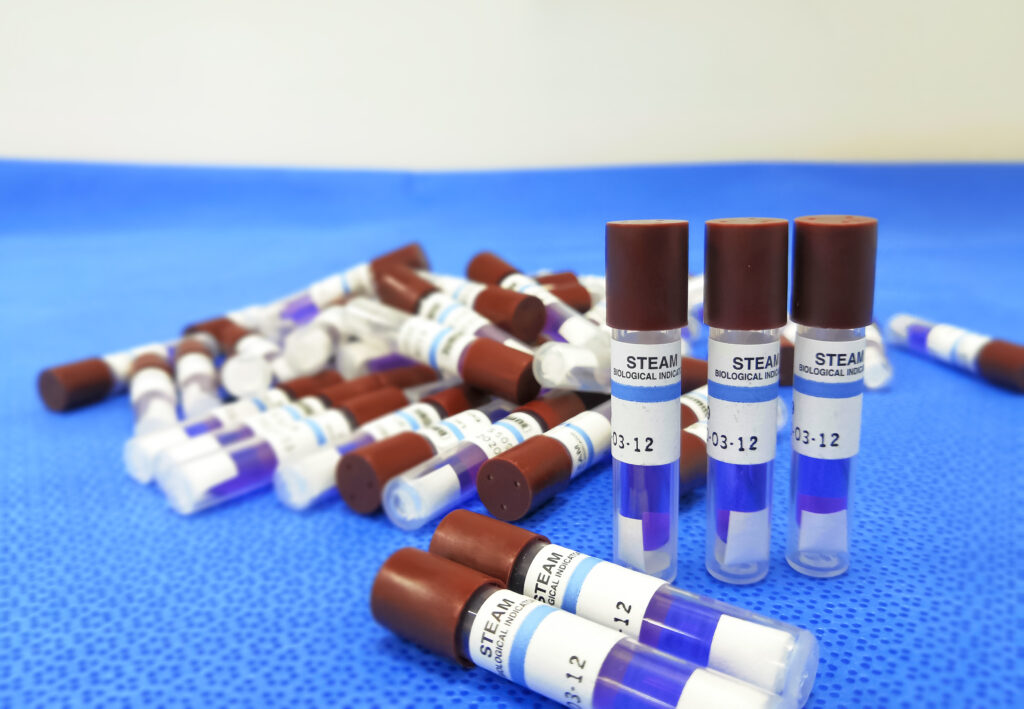
Biological Indicators (BI) containing specific resistant bacterium are one of the tools that have been developed to gauge the level of delivered lethality of a sterilization process. These BIs are designed to act as a surrogate for the native product bioburden present in and on products during validation and routine monitoring activities. A formal definition for BIs can be found in sterilization standards such as ANSI/AAMI/ISO 11138-7, Sterilization of Health Care Products – Biological Indicators – Part 7: Guidance for the Selection, Use, and Interpretation of Results.
BIs for use in sterilization validation studies should have the following characteristics:
Sterilization process validation in the simplest sense is generally achieved by establishing a linear death rate kinetic of the product’s bioburden when exposed to a specific sterilant. This facilitates the extrapolation of an exposure duration that will achieve the appropriate sterility assurance level (SAL). While the bioburden of the product can be used for this, it is not ideal. The native product bioburden is heterogenous in nature and can vary widely in population between different units of the same product making it an inconsistent measuring tool for SAL. BIs can be much more consistent but must be calibrated with regards to the average population per unit and resistance to the target sterilant.
Biological Indicator Population Verification
There are multiple methods for enumerating the population of a given BI. BI population enumeration can be conducted on individual BI units or as a group pooled together. A maceration technique may be ideal for substrates made of paper or material easily pulped in an aqueous buffer, but this may not work for other carriers. Solid carriers, for instance, might be better tested using more aggressive physical agitation via vigorous vortexing supplemented with glass beads or ultrasonication. The resulting spore suspension should be heat shocked to assist with spore germination for the most accurate count. A good measure of BI lot quality is checking the difference between a heat shock and non-heat spore count. If the data reveals a lower population in the heat shocked suspension, this may be an indicator that sporulation was not completed across the entire population. Alternatively, a lower population in the heat shocked suspension may indicate the heat treatment alone was sufficient to be lethal to a certain portion of the population. If the data indicates a higher population in the heat shocked suspension, this may indicate that the vegetative population was induced into sporulation in a more synchronous manner which would result in healthier spore coats that help to maintain BI resistance over a longer shelf-life period.
BIER Units and D-Values
Calibration of BI resistance is typically described as a decimal reduction value or D-value. Its definition is the amount of time, under a specific set of lethal conditions, required to reduce the BI population by one base 10 logarithm value. One method of determining the D-value of a particular BI is through the use of specifically engineered equipment known as a biological indicator evaluator resistometer (BIER). Each BIER unit is calibrated for use with a specific sterilization modality, whether that be ethylene oxide, moist heat, dry heat, or vaporized hydrogen peroxide (VHP). LexaMed has a moist heat BIER unit in house which can be used to determine a BI’s D-value and z-value using methods in compliance with ANSI/AAMI/ISO 11138-3, Sterilization of Health Care Products – Biological Indicators – Part 3: Biological Indicators for Moist Heat Sterilization Processes.
Creating the exposure conditions as rapidly as possible is crucial to determining an accurate D-value that may be reproducible over the shelf-life of the BI and for comparison to other BI lots as a quality control measure. To minimize the lag time to achieve constant exposure conditions and the come-down lag time, special equipment is required. A biological indicator evaluator resistometer (BIER) unit is specifically engineered to rapidly create the temperature, pressure, humidity, etc. as pertinent to the sterilant desired. ANSI/AAMI/ISO 18472, Sterilization of Health Care Products – Biological and Chemical Indicators – Test Equipment provides specific performance requirements for ethylene oxide, moist heat, dry heat, and VHP BIER units. LexaMed maintains a validated steam BIER operating at 110 °C to 140 °C in compliance with ANSI/AAMI/ISO 18472.
There are a few methods for calculating D-values. Most recognized are outlined in ANSI/AAMI/ ISO 11138-1, Sterilization of Health Care Products – Biological Indicators – Part 1: General Requirements. Most direct is the survivor curve method. It is conducted by utilizing a series of exposure times producing 100% survivors of the BI sample set. A plot of the log10 transform of the surviving population vs. exposure time produces a rectilinear curve or basically a straight line. The negative reciprocal of the line’s slope is the D-value, stated as the time to reduce the BI population by a factor of 10. There are alternative methods that use an estimation for spore survival after longer exposure times that result in the BI being potentially dead or viable. These D-value calculation methods use quantal survival data in an exposed BI set and are known as fraction-negative methods.
When selecting a BI for your sterilization process, you’ll want to compare the relative resistance of the BI and the native product bioburden. This can be done by running a fractional or sublethal sterilization cycle followed by tests of sterility. If there are a greater number of positive test samples for the BI compared to the product, the BI is considered to have a greater resistance to the sterilization process than the native bioburden and may be an acceptable choice for use in a sterilization validation.
Final Thoughts
Sterilization validation extends far beyond meeting regulatory expectations, it is a rigorously controlled scientific discipline where accuracy, reproducibility, and process understanding are essential. Biological Indicators serve as a critical tool in this effort, delivering a quantifiable and consistent measure of sterilization effectiveness across multiple modalities. Proper organism selection, carrier design, population verification, and D-value determination all contribute to the development of a reliable and defensible validation strategy.
At LexaMed, we recognize that effective sterilization validation requires more than standard solutions. Our team brings deep expertise in Biological Indicator development, customization, and performance verification supporting validation studies that reflect real-world manufacturing conditions. From early-stage cycle development to process optimization and regulatory rediness, we provide the scientific insight and laboratory capabilities needed to move your program forward with confidence.
If you are advancing a new sterilization process, addressing performance concerns, or evaluating the appropriate Biological Indicator for your application, contact us at [email protected]
LexaMed is ready to partner with you to help ensure your sterilization processes are compliant and scientifically sound.
Copyright @ 2025 LexaMed. All Rights Reserved